Russell Pecoraro, MD & J. Parker Dupree, MD
What is the Retina?
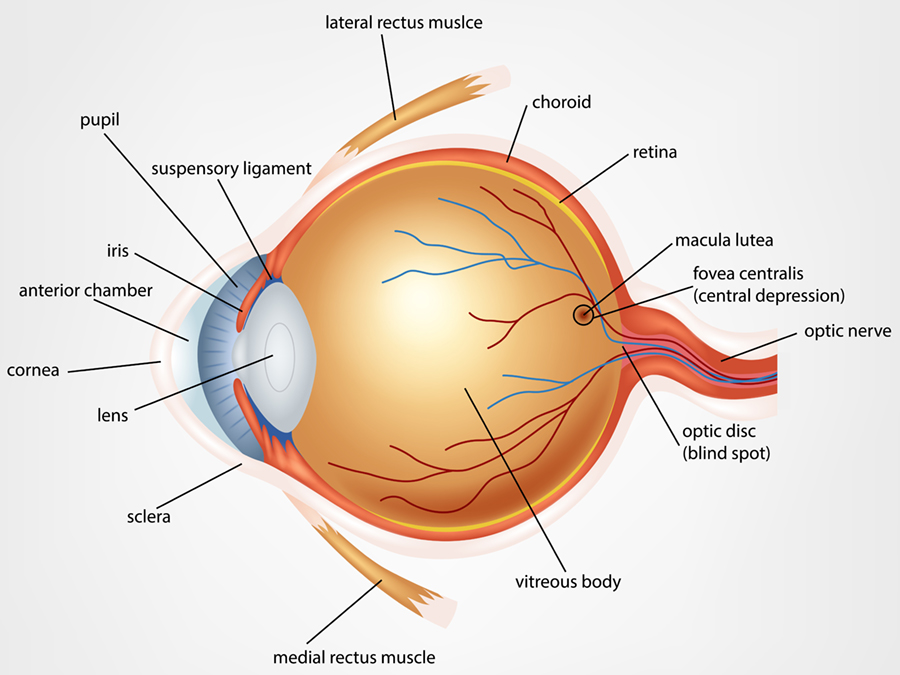
The retina is a thin layer of light-sensitive nerve cells that line the back of your eye. It’s part of the central nervous system and links to the brain through the optic nerve. Specialized photoreceptor cells, called rods and cones, receive the light that travel through your pupil and the lens of your eye onto your retina. Other neurons of the retina then convert the light into electrical impulses that travel along the optic nerve to a portion of your brain that translates the signals and provides images you can recognize. This necessary interaction between light and vision is why it’s harder to see at night or in a darker environment.
What Else is Part of the Retina?
The retina is fairly small, but it contains several components that are essential for clear vision. Along with the specialized photoreceptor cells, the retina includes the:
- Peripheral retina, which provides side vision and night vision
- Macula, a small area at the center of the retina that provides central or “straight-ahead” vision
- Fovea, a small depression in the center of the macula where eyesight is sharpest
A gel-like fluid called the vitreous humor fills the eye cavity that houses the retina, and small blood vessels supply necessary oxygen and nourishment to the tissue structures.
Damage to any part of the retina through injury or disease can affect retinal health and the clarity of vision it provides.
Macular Degeneration
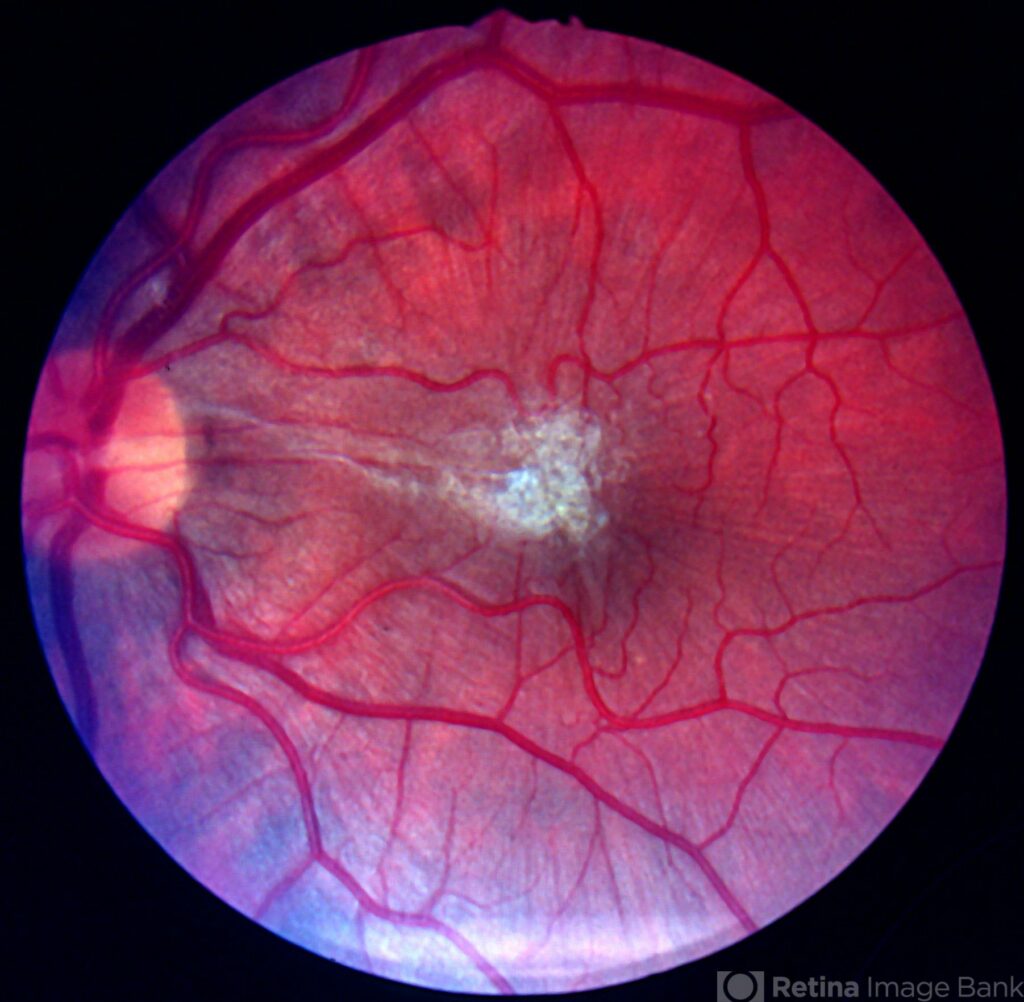
Macular Degeneration is one of the leading causes of vision loss for those 55 and older, and one of the most common eye diseases treated by the physicians at Clay Eye.
The macula is responsible for central vision in the eye, allowing the ability to read, drive a car, recognize faces or colors, as well as recognize fine detail. Macular Degeneration can destroy sharp central vision and is the leading cause of legal blindness.
In some individuals, tiny dot-like deposits, known as drusen, slowly accumulate beneath the macula. While these deposits usually do not cause visual loss directly, they indicate that a person is at risk for developing further problems with the macula. Atrophic or thin areas can develop in the macula which can lead to visual loss in the “dry” form of macular degeneration. In some patients, abnormal blood vessels may develop under the macula leading to the “wet” form of macular degeneration. If these vessels can be identified at an early stage, it may be possible to seal them with an injection of medications developed for wet macular degeneration or other treatments. If you notice any new distortion or visual changes, it is critical to contact your eye care provider immediately.
Cystoid Macular Edema (CME)
Cystoid Macular Edema (CME) is a condition in which the macula develops microscopic swelling which can blur the central vision. CME most commonly develops following intraocular surgery but may be associated with a variety of vascular conditions such as macular degeneration, diabetic retinopathy or vascular occlusion. Treatments for CME depend on its cause. CME may be treated with medicated eye drops, injected medication, laser treatments or surgery.
Diabetic Retinopathy
Diabetic retinopathy, is an eye condition that can cause vision loss and blindness in people who have diabetes. Over half of all Americans diagnosed with diabetes develop diabetic retinopathy.
Diabetic retinopathy occurs when tiny blood vessels in the retina (the light-sensitive layer of tissue in the back of your eye) become damaged and begin to leak fluid or blood resulting in blurred vision. Some patients may develop poor retinal circulation leading to abnormal blood vessel formation which can cause intraocular bleeding or retinal detachment.
If you have diabetes, it is important for you to monitor your glucose levels and get a comprehensive dilated eye exam once a year. The best prognosis for diabetic retinopathy is early detection and treatment.
Epiretinal Membranes (Macular Puckers)
An epiretinal membrane, commonly called a macular pucker, is a thin film-like covering that can develop over the central retina known as the macula. This area of the retina is responsible for your clear central vision. Epiretinal membranes may lead to blurry or distorted vision. Some epiretinal membranes require vitrectomy surgery with removal of the membrane for improvement of vision.
Flashes and Floaters – Posterior Vitreous Detachments
Flashes of light and floaters in the field of vision occur in healthy people, however, may also be a sign of serious problems. If flashes occur suddenly, it may be a sign that you have a torn retina.
Floaters, usually due to a posterior vitreous detachment, are caused by particles that are floating in the vitreous gel and cast shadows on the retina. As you age, floaters may naturally appear. However, if floaters occur suddenly, it may also be a sign that you have a torn retina.
If you experience sudden onset of either flashes or floaters, you should contact your doctor immediately.
Macular Holes
Macular holes are just that, holes in the macula. The macula is the central portion of the retina that is responsible for clearly seeing fine details.
A macular hole commonly affects people over the age of 55. As we age, the vitreous (the gel that fills up the inside of the eye) can shrink or condense and pull away from the retina, sometimes creating a macular hole in the process.
Many macular holes are treatable with vitrectomy surgery.
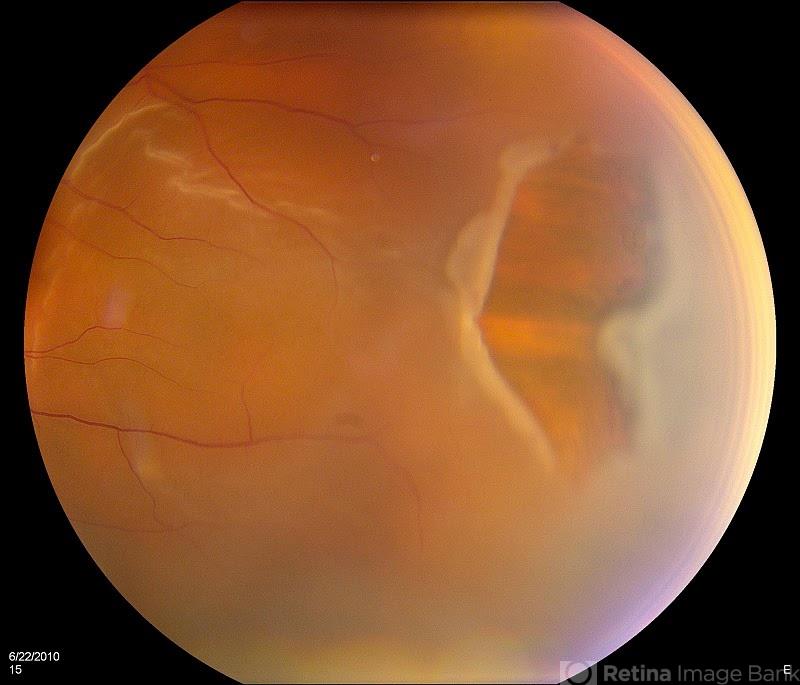
Retinal Tears and Detachment
Retinal Detachment and Retinal tears occur when the vitreous, a clear jelly-like substance that fills the eye, pulls from the retina and causes the retina to tear. The liquid that passes through the tear and settles under the retina results in separation of the retina from the back wall of the eye. The condition is termed a retinal detachment. An untreated detached retina frequently causes blindness.
You should contact your doctor as soon as you develop the symptoms of retinal detachment. Symptoms include seeing flashing lights, new floaters, or a gray curtain move across your field of vision.
RETINAL VASCULAR DISEASES
Retinal vascular diseases are common in people with high blood pressure, diabetes, and other factors that cause vascular disease throughout the body such as increasing age, high cholesterol, smoking, and hypertension. Retinal vascular diseases include retinal arterial macro aneurysm, retinal branch, and central artery and vein occlusion, diabetic retinopathy, and ocular ischemic syndrome. In simple terms, these are conditions that can restrict the blood flow throughout your eye structures and lead to vision loss or blindness. Our experienced Retina team coupled with our state-of-the-art diagnostic capabilities will help you manage your retinal eye condition.
Treatments
Steroid Injections/Anti-VEGF Injections
- Avastin
- Eylea
- Vabysmo
- Lucentis
The drugs listed above are various treatment options for age-related macular degeneration and retinal vascular diseases (blood vessel blockages including diabetic retinopathy). These agents work to block the growth of new blood vessels that may leak and contribute to vision problems. They are injectable medications that block the effects of Vascular Endothelial Growth Factor (VEGF) which is responsible for the growth of new blood vessels in the eye. VEGF is implicated in the development and progression of wet macular degeneration, diabetic retinopathy, and macular edema. VEGF promotes the growth of new abnormal blood vessels and increases the permeability of existing vessels leading to leakage. By blocking VEGF, Avastin and Lucentis can, in some cases, improve outcomes in patients with a broad variety of retinal and macular diseases.
Laser Treatment for Diabetic Retinopathy
Depending on the type of retinopathy you have, your doctor may recommend laser treatment. Laser treatment can be used to help reduce the swelling in your retina caused by leaky blood vessels. It can also be used to treat a more aggressive form of retinopathy, called “proliferative,” which can lead to bleeding into your eye, retinal detachments and loss of vision.
Laser Surgery for Retinal Tears
Once a retinal tear or hole is identified and determined to be threatening to your vision, it is important to have it repaired prior to it progressing to a retinal detachment. A laser beam is focused on the area surrounding the tear, and small microbursts of the laser are emitted sealing off the tear to prevent it from spreading.




