Macular Degeneration

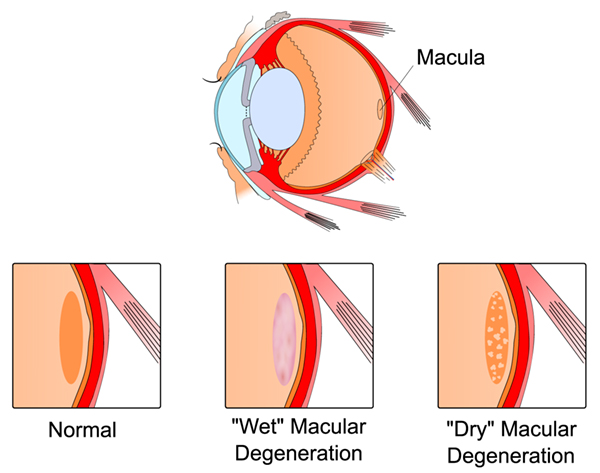
Macular degeneration is an age-related condition and is the most common cause of vision loss in people age 55 and older. The macula, the center of vision in the retina, is damaged as the disease develops. Macular degeneration can occur in two different forms, either “wet” or “dry”. The dry type, the most common form, occurs when the tissue in the macula thins and ceases to function properly. The wet type occurs when blood vessels grow and leak, causing swelling and scarring, which can lead to a loss of central vision.
Decreased function of the central retina occurs with macular degeneration causing vision to become hazy or blurry. Straight lines may appear wavy; objects may appear as the wrong shape or size, and it may become increasingly difficult to see objects up close. Macular degeneration increases with age, but other factors such as smoking, family history, gender, and high cholesterol may accelerate the condition.
Currently, there is no cure for macular degeneration, but there are certain treatments available to slow or stop the disease from progressing. Changes in diet and vitamin intake may slow dry macular degeneration. Wet macular degeneration can be treated through laser treatments and photodynamic therapy; both designed to close off the blood vessels causing the wet macular degeneration. Patients may regain a little vision through these treatments; but once vision is lost, it is very hard to restore.
What is Age-Related Macular Degeneration?
Age-related macular degeneration (AMD) is a disease of the retina. End-Stage AMD is the most advanced form of the disease and the leading cause of irreversible vision loss and legal blindness in individuals over the age of 65.
In early, less advanced AMD, visual symptoms are generally mild and may or may not impact vision-related activities. However, advanced stages of AMD can result in severe loss of sight in the central part of vision. This is often referred to as a central vision “blind spot.” This blind spot is different than the visual disturbances experienced with cataracts (clouding of the eye’s lens) and is not correctable by cataract surgery or eyeglasses. Side vision, or peripheral vision, is not affected by AMD but is too low resolution to make up for lost central vision. At this time, there is no cure for End-Stage AMD and no way to reverse its effects.
What is CentraSight® and the Telescope Implant?
The CentraSight treatment program uses a tiny telescope, an FDA-approved medical device, which is implanted inside the eye to improve vision and quality of life for individuals affected by End-Stage AMD. The telescope implant, about the size of a pea, is intended to improve distance and near vision in people who have lost central vision in both eyes because of End-Stage AMD. The telescope implant is surgically placed inside one eye. The implanted eye provides central vision; the other eye provides peripheral vision. The telescope implant is not a cure for End-Stage AMD. It will not restore your vision to the level it was before you had AMD, and it will not completely correct your vision loss. Patients with this level of AMD have had to cease driving due to their vision; after the telescope procedure, although near and distance vision may improve, driving will not be possible because the implant does not restore normal vision.
Am I a Candidate?
In general, to be considered a potential candidate for the telescope implant an ophthalmologist must first confirm that you:
- Have irreversible, End-Stage AMD resulting from either dry or wet AMD
- Are no longer a candidate for drug treatment of your AMD
- Have not had cataract surgery in the eye in which the telescope will be implanted
- Meet age, vision, and corneal health requirements
After the ophthalmologist confirms that you are a potential candidate, your vision will be tested using an external telescope simulator. The results of the test and visual training/rehabilitation evaluation visits will help you and your ophthalmologist decide if you are likely to benefit from the CentraSight treatment program. If so, the tests will also help you and your ophthalmologist discuss which eye should be treated and what your vision may be like after the treatment. Call us today to see if this procedure is right for you. Additional information can be found www.CentraSight.com.
The CentraSight treatment program involves four steps that start with diagnosis and continue after surgery.
Step 1: Diagnosis
Step 2: Candidate Screening
Step 3: Surgical Procedure
Step 4: Learning to Use Your New Vision
A member of your CentraSight team is involved at each step of the treatment. All CentraSight team members are highly qualified professionals, with special training in the CentraSight treatment program and the telescope implant technology. The following pages explain what you can expect at each step of the program.
The telescope implant is not a cure that “sees” for you. For the telescope implant to work for you, you will need to work with low vision specialists as well as practice on your own at home.
Realistic Goals:
- Recognizing the faces of family and friends
- Watching television
- Reading
- Various hobbies like painting, knitting or gardening
Unrealistic Goals:
- Driving
- Seeing a golf ball in flight
- Playing tennis
- Never having to use a magnifying glass again
Visual goals can be assessed with an external telescope simulation during pre-surgery screening visits.
Your ophthalmologist will describe the risks and benefits of the telescope implant to you, including the risks of surgery.
Step 1: Diagnosis

CentraSight Team Member: Retina Specialist/Dr. Pecoraro
To be considered as a possible candidate for the treatment, you must first be examined by Dr. Pecoraro, our retina specialist, to confirm that you have End-Stage AMD. This will involve a thorough medical eye examination and a review of your medical history, including any conditions that may make the procedure difficult for you or increase the likelihood of complications. Dr. Pecoraro will explain the benefits and risks of the CentraSight treatment program and answer any questions you may have.
Step 2: Candidate Screening
CentraSight Team Members: Retina Specialist/Dr. Pecoraro, Low Vision Optometrist,
Low Vision Occupational Therapist
The screening includes several appointments and a low vision evaluation performed by a low vision optometrist. The candidate screening step includes testing your vision using external telescope simulators. The results of these tests can help give you and your CentraSight Team a good idea of what your vision may be like after the telescope implantation surgery and if the effect of the magnification in one eye will be useful to you. Low vision providers will also talk to you about how your new vision status may affect your everyday life and how following a visual training/rehabilitation program after surgery will help you reach your vision goals.
Step 3: Surgical Procedure
CentraSight Team Member: Cornea/Cataract Surgeon/Dr. Downer
The telescope implantation surgical procedure is performed on only one eye. It involves removing the eye’s natural lens and replacing it with the tiny telescope implant. The surgical procedure is relatively short (1-1.5 hours) and is performed by a specially trained ophthalmologist. You won’t have to stay in a hospital and will return home the same day. The telescope is virtually unnoticeable to others because it is implanted totally inside the eye, and mostly covered by the colored portion of the eye (iris).
What to Expect with the Surgical Procedure
Before the Surgery
Before the surgery, your surgeon will take your medical history and check the health of both of your eyes. You should let your surgeon know if you take any medication or have any allergies. Be sure to discuss all your questions with your surgeon before scheduling your surgery. You will need to arrange for transportation to and from your surgery appointment.
Day of Surgery
The procedure is performed on an outpatient basis and generally takes 1-1.5 hours. The surgery involves several steps:
- Your eye will be numbed at the beginning of the procedure so you will not feel any pain
- Special eye drops will be administered to temporarily enlarge your pupil
- Dr. Downer will remove your eye’s natural lens
- The telescope implant will be placed in the same position where the natural lens was located
- The surgical incision will be sutured closed
If Dr. Downer is unable to implant the telescope during surgery, he will implant a standard intraocular lens (IOL), as in any procedure for cataract removal.
- After the Surgery
- After surgery, you will have follow-up visits with your Dr. Downer. You will have to take eye drops for several weeks.
- You should expect a gradual improvement in your vision of the treated eye to occur over a period of time, ranging from weeks to months.
- If you are found to be a candidate, your surgeon will provide you more detailed information about the procedure and potential risks.
Step 4: Learning To Use Your New Vision
CentraSight Team Members: Low Vision Optometrist, Low Vision Occupational Therapist
After you have recovered from surgery, specially trained low vision optometrists and occupational therapists will work with you to prescribe eyeglasses and complete your rehabilitation to help you adapt and learn how to use your new vision in daily life. They will work with you on an individualized plan over several weeks to reach your personal goals.
What are the Benefits of the Telescope Implant?
The effectiveness of the telescope implant has been demonstrated in FDA approved studies. In results from a survey in the FDA clinical trial, patients who received the telescope implant generally reported that they were less dependent on others, less frustrated and worried about their vision, less limited in their ability to see, and better able to visit with others and recognize facial expressions/reactions. Overall, the survey findings showed patients had a clinically important improvement in the quality of life.
An FDA study found that nine out of ten patients with the telescope implant improved vision by at least two lines on the eye chart. 1
What are the Risks of the Telescope Implant?
As with any medical intervention, potential risks and complications exist with the telescope implant. The most common risks of the telescope surgery include inflammatory deposits on the device and increased pressure in the eye. Significant adverse events include corneal swelling, corneal transplant, and a decrease in visual acuity. There is a risk that having the telescope implantation surgery could worsen your vision rather than improve it. Individual results may vary. You should talk to your doctor about these and other potential risks to find out if the telescope implant is right for you. Additional information can be found at www.CentraSight.com.
1. Hudson HL, et al. Ophthalmology. 2006.
